C-PLGD is a rare autosomal recessive multisystem disorder of the fibrinolytic system. Mutations in the PLG gene result in extravascular fibrinous deposits, termed ligneous for their woody appearance, that accumulate on mucous membranes such as the conjunctiva and airways, with resultant tissue injury or organ dysfunction. Ligneous conjunctivitis (LC) is the most common manifestation (> 80%) of C-PLGD. Ligneous lesions affecting the respiratory system have been reported in 20% of patients in a large case series (Schuster et. al. JTH 2007). We report 3 new cases in addition to a previously reported case of airway obstruction with respiratory distress successfully treated with intravenous Glu-plasminogen concentrate (Human) (IV-PLG).
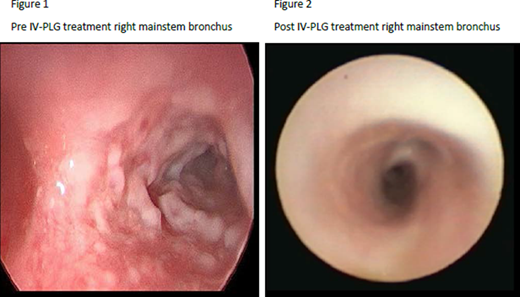
Case 1: A 16-month-old female with C-PLGD, with onset of LC at 3 weeks of age, developed a febrile illness with upper respiratory tract symptoms and exacerbation of LC. Four weeks after the exacerbation presented, she developed wheezing unresponsive to bronchodilator and corticosteroid treatment. She progressed to stridor, tachypnea and hypercapnia and was treated with fresh frozen plasma (FFP) infusions. She underwent a bronchoscopy which revealed friable airways and fibrinous lesions in the right mainstem bronchus (Figure 1). Computed tomography (CT) of the chest revealed airway narrowing (R>L) with distal air trapping. She was admitted to the pediatric intensive care unit (PICU) for monitoring and continued FFP treatment every 12 hours without relief. Compassionate use of IV-PLG was requested and she initiated urgent treatment under an expanded access protocol. Significant improvement in stridor and tachypnea occurred within 48 hours of starting therapy and was discharged from the PICU after 2 weeks without symptom recurrence. 10 days post treatment repeat bronchoscopy showed improvement in obstructing airway lesions (Figure 2), and CT scan revealed improvement in airway narrowing and air trapping. She is currently continuing treatment administered every 5 days.
Case 2: A 16-month-old male with C-PLGD and shunted congenital hydrocephalous, presented with worsening LC (onset at 7 months) and hoarseness from suspected ligneous airway disease. He was admitted to the PICU for monitoring, supplemental oxygen therapy for hypoxemia, and FFP infusions every 12 hours with only minimal relief. Chest CT revealed bronchiectasis and possible airway lesions. IV-PLG compassionate use was requested; he initiated urgent treatment under an expanded access protocol. Four days after starting treatment he underwent bronchoscopy confirming airway ligneous involvement, and ophthalmologic membranes were also stripped. He responded to treatment with improvement of both respiratory and eye symptoms without further requirement for supplemental oxygen; he was discharged from PICU after 8 days total, and 6 days after starting IV-PLG. His eyes healed without lesion recurrence. He continues to receive IV plasminogen replacement infusions every 5 days.
Case 3: A 3-year-old C-PLGD male, diagnosed at 7 weeks of age with LC, developed an upper respiratory infection with persistent hoarseness over a 3-week period. Due to potential airway involvement concern, he underwent upper airway laryngoscopy; a right vocal cord small polyp and a papillomatous mass noted below vocal cords were observed. Compassionate use of IV-PLG was requested; he initiated urgent treatment under an expanded access protocol. The patient experienced resolution of hoarseness in 4 weeks, with significant improvement in his LC. He has had no further clinical respiratory symptoms or LC exacerbations and is currently continuing treatment administered every 5 days.
Plasminogen replacement has previously been reported in a fourth C-PLGD pediatric patient (22-month-old male) who had experienced cardiopulmonary arrest due to airway obstruction (Hassenpflug et. al. Blood 2016). This patient required ongoing ventilator support; treatment with IV-PLG assisted in weaning from ventilator support. These cases demonstrate the potential role for IV-PLG treatment in C-PLGD patients with airway obstruction due to fibrinous lesions, to prevent progression of obstruction resulting in respiratory failure; additional controlled studies would need to be performed to further support these observations.
Nakar:Prometic Biotherapeutics: Research Funding; Kedrion SpA: Research Funding. McDaniel:Prometic Biotherapeutics: Consultancy, Other: Investigator Clinical Trial. Parker:Liminal BioSciences: Current Employment, Current equity holder in publicly-traded company. Trybul:Liminal BioSciences: Current Employment, Current equity holder in publicly-traded company. Shapiro:Sangamo: Research Funding; ProMetic Bio Therapeutics: Consultancy, Research Funding; Pfizer: Research Funding; Octapharma: Research Funding; OPKO: Research Funding; Novo Nordisk: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Novartis: Research Funding; Kedrion Biopharma: Research Funding; Glover Blood Therapeutics: Research Funding; Genentech/Roche: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Daiichi Sankyo: Research Funding; Catalyst BioSciences: Membership on an entity's Board of Directors or advisory committees; BioMarin: Research Funding; Bioverativ: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Takeda: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novo Nordisk Hemophilia Foundation: Membership on an entity's Board of Directors or advisory committees; Sigilon: Consultancy, Membership on an entity's Board of Directors or advisory committees; Agios: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal